Integrated Architectures for Predicting Hospital Readmissions Using Machine Learning
Keywords:
hospital readmission prediction, machine learning architecture, predictive modeling, real-time data processing, post-discharge care management, healthcare analytics, personalized interventionsAbstract
Objective: This study proposes a robust architecture that integrates machine learning models for predicting hospital readmissions within 30 days of discharge. The architecture aims to enable proactive interventions, personalized post-discharge care planning, and integration with existing hospital workflows to improve patient outcomes and reduce readmission rates.
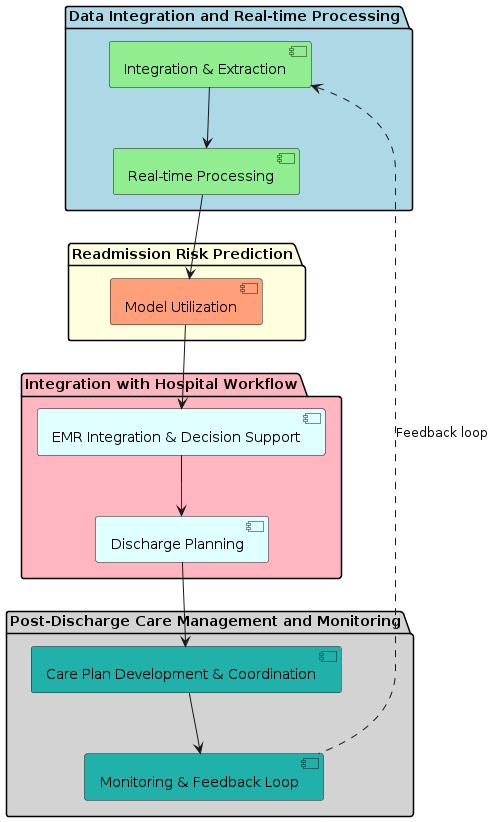
Methods: The proposed architecture includes a data integration layer that extracts and preprocesses patient data from EHR and other systems. Various machine learning classifiers are trained and evaluated using the preprocessed data, with feature selection and hyperparameter tuning employed to optimize performance. The trained models are integrated into the hospital's real-time data processing pipeline for risk prediction, and the predicted scores are incorporated into clinical decision support systems and EMR. Personalized care plans are developed for high-risk patients based on the predicted readmission risk scores. The architecture also includes a continuous monitoring and improvement loop to track performance metrics, collect feedback, and periodically retrain and update the models.
Results: Experimental results demonstrate the potential of the proposed architecture. Initial experiments showed moderate performance across classifiers, with accuracies ranging from 0.715 to 0.809. Recall for the positive class (readmitted patients) was low. After hyperparameter tuning, KNN achieved an accuracy of 0.833, while Naive Bayes and Adaboost classifiers significantly improved recall for the positive class (0.898 and 0.998, respectively) at the cost of reduced accuracy. XGB and Gradient Boosting classifiers showed slight improvements in accuracy and recall after tuning.
Conclusion: The architecture enables proactive identification of high-risk patients, personalized interventions, and continuous improvement based on model performance and feedback. The experimental results demonstrate the strong performance of the predictive models. Additional verification is necessary to verify the effectiveness of the complete architecture in reducing readmissions and enhancing patient outcomes in real-world healthcare contexts. The architecture aims to serves as a blueprint for implementing data-driven readmission prediction and proactive care management in hospitals.